- Home
- Users & Science
- Scientific Documentation
- ESRF Highlights
- ESRF Highlights 2009
- X-ray imaging
- Methacholine and ovalbumin airway challenges assessed by synchrotron lung imaging
Methacholine and ovalbumin airway challenges assessed by synchrotron lung imaging
Asthma is one of the most common chronic inflammatory diseases of the airways of our lungs. It is characterised by airway hyperresponsiveness and severe airway narrowing leading to heterogeneous distal lung ventilation. Although several imaging modalities have demonstrated this heterogeneity both in human subjects and animal models, the mechanisms of such complex airway behaviour remain poorly understood. This is in part due to the lack of an ideal imaging technique.
Recently, we introduced a computed tomography (CT) technique for imaging lung function that combines both high spatial and temporal resolution, allowing for truly quantitative measurements of regional ventilation [1]. This technique has the ability to image both lung function and the underlying lung morphology simultaneously. It uses radiation from a synchrotron source, which, as opposed to standard X-ray sources, allows selection of a monochromatic X-ray beam from the full spectrum while conserving enough intensity for imaging. Stable Xe gas is administered as an inhaled contrast agent. Two images are acquired simultaneously using two energies that bracket the K-absorption edge of Xe, their subtraction yields the distribution of the Xe gas inside the lungs. One advantage of this so-called K-edge subtraction (KES) method over the CT techniques using standard X-ray sources is that it allows a direct quantification of the absolute density of the Xe gas at any given point in a lung CT image. Another advantage is that contrast resolution is markedly improved by avoiding non-selective contrast and beam hardening, which occurs with conventional X-ray sources. Moreover, both structural and functional images are obtained simultaneously. Sequential imaging using this technique allows the quantification of regional lung ventilation.
 |
|
Fig. 129: Mono-energetic CT images showing changes in the central airway cross-section at the different experimental stages in one representative animal. Magnification of the indicated square areas are shown in the upper right corners. |
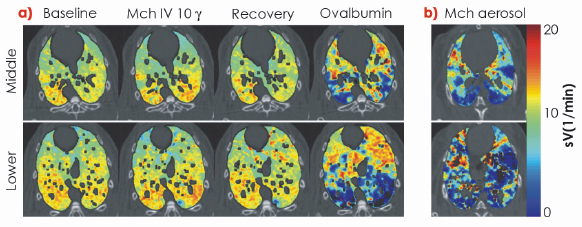
Computational models have shown that even for uniform smooth muscle activation of a symmetric fractal bronchial tree, the presence of minimal heterogeneity breaks the symmetry and leads to large clusters of poorly ventilated lung units [2]. The goal of the present study was to determine whether the mechanism of airway challenge is also involved in the heterogeneity of response in the bronchial tree. We characterised the changes that occur in the pulmonary system during a nonspecific challenge with methacholine (Mch), a substance acting on muscarinic receptors on airway smooth muscle cells causing constriction and following airway provocation with a specific allergen, ovalbumin (Ova) in sensitised rabbits. The functional changes were assessed by respiratory mechanical measurements allowing partitioning of the airway and tissue changes, based on the overall low-frequency impedance (Zrs) measurements of the respiratory system. We combined these results with those obtained with KES imaging, which allowed simultaneous measurements of the changes in the calibre of conducting airways and regional lung ventilation (Figure 129). Functional localisation of the primarily affected lung compartment revealed radical differences between the changes due to Ova and Mch provocation (Figure 130), despite similar magnitudes of increase in airway resistance (Raw). Our results demonstrate that through intravenous (IV) infusion, the effect of Mch in the lungs predominates in central airways, with minor changes in the lung periphery. In contrast, following Ova provocation through the same IV route, both the mechanical and the functional imaging parameters indicated the development of severe ventilation heterogeneity and airway closure in the lung periphery. Despite different underlying mechanisms, inhaled Mch induced a heterogeneous lung response similar to that observed with the IV allergen.
 |
|
Fig. 130: a) Images of specific ventilation in one representative sensitised rabbit at baseline, during methacholine (Mch) infusion, upon recovery and after Ova provocation; g: µg/kg/min, Ova: ovalbumin; b) images of regional ventilation in one representative control rabbit following Mch aerosol inhalation. Black colour indicates zero specific ventilation. |
In conclusion, in this study we found that the pattern of lung response caused by Mch, a non-specific stimulus, and Ova in a sensitised organism, in other words a specific stimulus, are fundamentally different through the IV route. Although inhaled Mch induced a heterogeneous lung response similar to that observed with the IV allergen, these similar patterns are due to different mechanisms. These findings suggest that both the mechanism and route of airway challenge play an important role in determining the heterogeneity of airway response. These findings may have important implications for further understanding of the disease mechanisms and drug-targeting strategies for asthma.
References
[1] S. Bayat et al., J Appl Physiol. 100, 1964-73 (2006).
[2] J.G. Venegas et al., Nature 434, 777-82 (2005).
Principal publication and authors
S. Bayat (a), S. Strengell (b), L. Porra (c,d), T.Z. Janosi (e), F. Petak (f), H. Suhonen (d), P. Suortti (c,d), Z. Hantos (f), A.R.A. Sovijärvi (b) and W. Habre (e), Am J Respir Crit Care Med. 180, 296-303 (2009).
(a) Université de Picardie Jules Verne, EA4285 Péritox-INERIS and CHU Amiens (France)
(b) Department of Clinical Physiology and Nuclear Medicine, Helsinki University Central Hospital (Finland)
(c) ESRF
(d) Department of Physics, University of Helsinki (Finland)
(e) Geneva Children’s Hospital, University Hospitals of Geneva and Geneva University (Switzerland)
(f) Department of Medical Informatics and Engineering, University of Szeged (Hungary)



