- Home
- Users & Science
- Scientific Documentation
- ESRF Highlights
- ESRF Highlights 2001
- Life Sciences
- The Weanling Piglet Cerebellum: a Surrogate for Tolerance to Microbeam Radiation Therapy in Pediatric Neuro-oncology
The Weanling Piglet Cerebellum: a Surrogate for Tolerance to Microbeam Radiation Therapy in Pediatric Neuro-oncology
Microbeam radiation therapy (MRT) is directed towards clinical applications. Theory and the rationale of preclinical experiments of MRT are based on dose-volume relationships that shape tissue complications after ionising irradiation. In general, the smaller the irradiated macroscopic tissue volumes, the higher the threshold absorbed doses for damage to normal tissues. Present-day clinical applications of this principle include stereotaxic radiosurgery and conformal radiotherapy, using photon beams collimated in millimetres.
Synchrotron radiation beams permit the production of microscopic beams that practically do not divergence within the tissues. After high-intensity X-ray wiggler beams with negligible divergence became available in the 1980s, dose-volume relationships were tested in the microscopic range, first at Brookhaven National Laboratory's (BNL) National Synchrotron Light Source. MRT was then implemented at the ESRF using an array of thin (20-30 µm), parallel, closely spaced microplanar beams from a multislit collimator installed at the ID17 beamline. The adult rat brain proved to be extraordinarily resistant to serious damage by MRT up to several hundred Gy, although some individual brain cells directly in the path of the microbeams were destroyed. Entrance doses of 10,000 Gy were required to destroy normal rat brain tissues.
Microplanar beams crossfired toward the target in parallel exposures at 100 µm intervals (entrance doses of 312 or 625 Gy) considerably extended the median survival time of young adult rats bearing advanced intracerebral gliosarcomas, ablating about half of them. Histopathologically recognisable loss of tissue was seen only within the cross-irradiated volume of the brain. In unidirectionally irradiated volumes of the brain, tissue damage was minor or nonexistent. The results suggested the possibility of a differential effect between normal and tumour tissue for microbeam irradiation. This biological selectivity is likely to be related to differences between vasculature in tumours and in normal tissues. The mechanisms are as yet unknown. A better understanding of the vascular events may require the use of a vasculature that can be observed in vivo, such as that of the chorio-allantoic membrane in fertilised chicken eggs. MRT at the ESRF and at BNL, using only one exposure to parallel microplanar beams was shown to be also palliative or curative in young adult rats bearing lethal intracerebral gliosarcomas.
MRT might be able to palliate brain tumors in human infants for whom seamless beams of radiation delivered conventionally may carry unacceptable risks of long-term neurological disability. The ultimate goal of radiotherapy is cessation of tumor growth without radiotoxic side effects. In practice, one uses the highest doses of radiation tolerated by vital tissues. We have studied the effect of therapeutic doses of microbeams delivered laterally, unidirectionally through the hindbrains of normal suckling rats about two weeks after birth. The combination of a high skin-entrance dose (150 Gy) and narrow intervals (105 µm midslice-to-midslice) between irradiated tissue microslices (width ~28 µm), in a relatively large (1 cm x 1 cm) swath of the hindbrain resulted in loss of cerebellar and body weight, as well as in neurological and behavioural dysfunction. Conversely, a significantly smaller effect was noted in rats that had been irradiated with a lower dose and/or wider beam spacing.
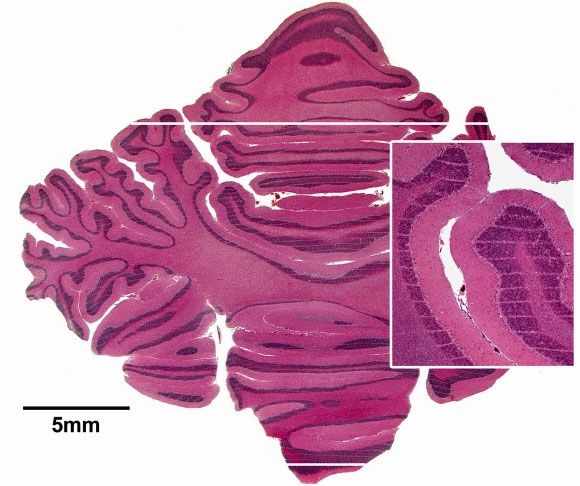 |
| Fig. 24: Cerebellum of a piglet ~15 months after irradiation (skin entrance dose: 300 Gy), stained horizontal tissue section. The tissue maintains its normal architecture. The thin white horizontal parallel stripes, clearly visible in the inset, correspond to the paths of the microbeams; the beam spacing was ~210 µm. Two thick white horizontal lines show the anteroposterior limits of the array of microplanes. |
The next step was to test tissue tolerance of the brain in larger animals. The cerebellum of the weanling piglet was used as a surrogate for the radiosensitive human infant cerebellum. Five weanlings in a 47-day-old litter of seven, and eight weanlings in a 40-day-old litter of eleven were irradiated at the ESRF. A 1.5 cm-wide x 1.5 cm-high array of microbeams was propagated horizontally through the cerebella of the prone, anesthetised piglets. Skin-entrance intra-microbeam peak absorbed doses were 150, 300, 425, or 600 Gy. For ~66 weeks (first litter; until euthanasia; Figure 24), or ~70 weeks (second litter) after irradiation, the littermates were developmentally, behaviourally, neurologically and radiologically (Figure 25) normal as observed and tested by experienced farmers and veterinary scientists unaware of which piglets were irradiated or sham-irradiated. These observations give credence to MRT's potential as an adjunct therapy for brain tumors in infancy.
 |
Fig. 25: Magnetic resonance image of the brain of a ~3 month-old piglet of the first litter; metric scale. No differences were apparent between irradiated piglets and sham-irradiated littermates. |
References
[1] J.A. Laissue, G. Geiser, P.O. Spanne, F.A. Dilmanian, J-O. Gebbers, M. Geiser,. X.Y. Wu, M.S. Makar, P.L. Micca, M.M. Nawrocky, D.D. Joel and D.N. Slatkin, Int. J. Cancer 78, 654-660 (1998).
Principal Publication and Authors
J.A. Laissue (a), H. Blattmann (b), M. Di Michiel (c), D.N. Slatkin (a), N. Lyubimova (a), R. Guzman (d), W. Zimmermann (e), S. Birrer (e), T. Bley (f), P. Kircher (e), R. Stettler (e), R. Fatzer (f), A. Jaggy (f) , H. M. Smilowitz (g), E. Brauer (c), A. Bravin (c), G. Le Duc (c), C. Nemoz (c), M. Renier (c), W. Thomlinson (c), J. Stepanek (b) and H-P. Wagner (a), in Medical Applications of Penetrating Radiation, H.B. Barber, H. Roehrig, F.P. Doty, R.C. Schirato, E.J. Morton (Eds.), Proceedings of SPIE 4508, 65-73, (2001).
(a) Institute of Pathology, University of Bern, (Switzerland)
(b) Paul Scherrer Institute (PSI), Villigen, (Switzerland)
(c) ESRF
(d) Neuroradiology Division, Inselspital, University of Bern, (Switzerland)
(e) Division of Porcine Diseases, Faculty of Veterinary Medicine, University of Bern (Switzerland)
(f) Division of Animal Neurology, Faculty of Veterinary Medicine, University of Bern (Switzerland)
(g) University of Connecticut Health Center, Connecticut (USA)



